Although the MSP historically required settling parties to notify Medicare of liability settlements with beneficiaries, Congress formalized reporting obligations under Section 111 of the Medicare, Medicaid, and SCHIP Extension Act of 2007.
How do I report a lawsuit settlement to Medicaid?
The first step would be reporting the receipt of the money to the SSI program. This must be done within 10 days of receiving the settlement. After reporting, it would be advisable to contact or consult a reputable service to handle the matter. Medicaid considers assets or money from a lawsuit settlement to be income for the month it was received.
Do lawsuit settlements affect Medicaid eligibility?
If the money from a lawsuit is paid on a monthly basis, then if the amount paid is more than their Medicaid benefit, they are likely to lose their benefit for the months they will receive payment from a lawsuit settlement. Lawsuit settlements affect Medicaid qualification one way or another.
How do Medicaid recipients spend personal injury settlements?
1. Spend Down: Medicaid recipients can spend their money (in the same calendar month personal injury proceeds become available to them). This typically makes the most sense for small personal injury settlements.
How long does it take for Medicaid to approve a settlement?
This must be done within 10 days of receiving the settlement. After reporting, it would be advisable to contact or consult a reputable service to handle the matter. Medicaid considers assets or money from a lawsuit settlement to be income for the month it was received.
Will a settlement affect my Medicare?
Since Medicare is an entitlement benefit and not a needs-based program, a client who receives legal settlement won't lose their Medicare benefits. It will not be impacted when a client receives a settlement.
What is the purpose of section 111 reporting?
The purpose of Section 111 reporting is to enable Medicare to correctly pay for the health insurance benefits of Medicare beneficiaries by determining primary versus secondary payer responsibility. Section 111 authorizes CMS and GHP RREs to electronically exchange health insurance benefit entitlement information.
What is the reporting process of CMS?
Reporting is accomplished by either the submission of an electronic file of liability, no-fault, and workers' compensation claim information, where the injured party is a Medicare beneficiary, or by entry of this claim information directly into a secure Web portal, depending on the volume of data to be submitted.
What is Medicare mandatory reporting threshold?
CMS has defined mandatory reporting thresholds solely for purposes of the required Section 111 Medicare Secondary Payer (MSP) reporting requirements. These thresholds are not exceptions for any other obligation or responsibility of any individual or entity with respect to the MSP provisions.
What is a responsible reporting entity?
Responsible Reporting Entity (RRE) — the party that is responsible for funding a claim payment to an individual eligible for Medicare benefits is considered the Responsible Reporting Entity (RRE) under the provisions of the Medicare, Medicaid, and SCHIP Extension Act (MMSEA) of 2007.
What is the Medicare Medicaid and Schip Extension Act of 2007?
The MMSEA substantially expands the federal government's ability to seek reimbursement of past and future Medicare payments in covered claims, including liability claims.
What is the minimum requirement for reporting data to CMS?
EHR Reporting Period in 2020 The EHR reporting period for new and returning participants attesting to CMS is a minimum of any continuous 90-day period, for both 2020 and 2021. Actions in the numerator and denominator of measures must be performed within a self-selected 90-day period in calendar year (CY) 2020.
Do Medicare benefits have to be repaid?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
What is an ODAG report?
Organization Determinations, Appeals and Grievances (ODAG) protocols help to evaluate performance in the areas outlined in the Centers for Medicare and Medicaid Services (CMS) Program Audit Protocol and Data Request related to Medicare Part C ODAG.
What is Medicare Secondary Payer recovery process?
Note: The Medicare Secondary Payer Recovery Portal (MSPRP) is a web-based tool designed to assist in the resolution of Liability Insurance, No-Fault Insurance, and Workers' Compensation Medicare recovery cases.
What does CMS stand for?
Centers for Medicare & Medicaid ServicesThe Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
What must be reported under the Sunshine Act?
Since Aug. 1, 2013, the Physician Payments Sunshine Act (Sunshine Act), requires manufacturers of drugs, medical devices, and biologicals that participate in U.S. federal health care programs to track and then report certain payments and items of value given to physicians and teaching hospitals.
How do I use CMS supervisor in Avaya?
0:0511:13How to log in and run reports using the Avaya CMS Supervisor Web ...YouTubeStart of suggested clipEnd of suggested clipYou will log in to CMS supervisor web using your standard web browser the URL is HTTP colon slashMoreYou will log in to CMS supervisor web using your standard web browser the URL is HTTP colon slash slash the hostname or IP address of the CMS server colon.
Who is reported on the Sunshine Act?
The Physician Payments Sunshine Act (42 U.S.C. & 1320a -7b) requires manufacturers of drugs, medical devices, biologics, and medical supplies and group purchasing organizations (GPOs) to report to the CMS services payments made and investment interests given to physicians and teaching hospitals.
Who manages Medicaid funds?
A trustee – usually a family member or trusted friend (in a d4A special needs trust) or professional trustee (in a d4C special needs trust)manages the money and can only distribute money to pay for services and products not currently provided by Medicaid.
How to spend Medicaid money?
This typically makes the most sense for small personal injury settlements. They are free to buy clothing, pay off credit card debts or other loans, buying a big-screen TV, going out to a nice dinner, travel expenses, making repairs to the home or car, and more. As long as they can spend the amount (over $2,000) in the same calendar month in which it is received, they can report same to DCF/SSA and retain their Medicaid benefits.
Why must a client inform DCF and SSA?
The reason why your client must still inform DCF and SSA because if they fail to report the new asset you have provided to them through their personal injury case, and they unwittingly continue to receive benefits when they are no longer eligible, Medicaid will eventually find out and send the former Medicaid recipient a bill, demanding to be reimbursed for funds that Medicaid should not have paid during months eligibility was lost.
What is the Medicaid asset test in Florida?
Florida Medicaid Asset Test. The asset test just says that a Medicaid recipient cannot have more than $2,000.00 in combined countable assets. There are a few items that are usually not countable by Medicaid: the most typical of the excluded / non-countable assets are: the value of the homestead and one car.
What is Medicaid 101?
But, first, a quick Medicaid primer: Medicaid is a means-tested program – meaning that in order to receive Medicaid an individual must meet Medicaid’s low income and asset tests.
Where to fill out SSA 8150-EV?
SSA-8150-EV must be filled out and sent to the SSA district office associated with the client's zip code (if on a Medicaid program associated with Social Security Income (SSI).You can use the Social Security office locator by clicking on the link and entering your zip code.
Can a medical malpractice lawyer help with Medicaid?
A Medicaid -planning lawyer will have other creative ways of protecting medical malpractice or personal injury settlement in order to maintain Medicaid eligibility, but this provides some basic information of what you should bethinking about to preserve Medicaid benefits after a personal injury client receives their portion of the financial recovery.
What is the CMS inquiry system?
CMS will establish a "query access" system to assist RREs in determining whether a claimant is entitled to Medicare benefits. Starting July 1, 2009, a registered RRE (or its designated agent) will be able to inquire, and Medicare will confirm, whether a claimant is a Medicare beneficiary. CMS will process one inquiry per month (which may include numerous claimants) per RRE ID.
What is MMSEA 111?
Briefly, Section 111 of MMSEA requires businesses paying personal injury settlements or judgments to a claimant to determine whether a claimant is entitled to Medicare benefits and, if so, report information about the payment to CMS in electronic format.
When are RRE reports due?
Given the upcoming RRE registration period of May 1 to June 30, 2009, and the mandatory initial reports coming due in the fourth quarter of 2009, businesses defending personal injury and wrongful death lawsuits and claims should inform themselves now about the new requirements and, if applicable, implement procedures to comply with the law. With penalties of $1,000 per day per claimant for failure to report payments to Medicare beneficiaries, businesses simply cannot afford to ignore the requirements of MMSEA Section 111.
When is MMSEA 111 effective?
For self-insured businesses, as that term is defined above, the effective date for these new requirements is July 1, 2009. However, advance planning and action will be required by these businesses well before that date.
Does RRE have to use an agent?
Once the RRE has registered, it may utilize an agent for submission of its subsequent required reports. Designation of an agent does not shift to the agent the RRE's reporting responsibility; the RRE remains solely responsible and accountable for complying with CMS instructions for implementing Section 111 and for the accuracy of data submitted by the agent.
What is the 2009 User Guide?
The March 16, 2009 User Guide provides detailed amplifying and clarifying information regarding reporting requirements. A few of the requirements are worth highlighting here:
Can Medicare pay medical expenses?
If Medicare pays medical expenses that should have been paid by a "primary plan," Medicare is entitled to recover those payments from the "primary payer" and from "an entity that receives payment from a primary payer." Until 2003, most courts considering Medicare reimbursement lawsuits ruled that Medicare was permitted to recover only from insurers, not tortfeasors that settle with and pay claimants from their own funds. But in 2003, Congress amended the Medicare as Secondary Payer Act (MSP) to expand the definition of the term "self-insured plan," specifying that any "entity that engages in a business, trade, or profession shall be deemed to have a self-insured plan if it carries its own risk (whether by a failure to obtain insurance, or otherwise) in whole or in part ." Construing the 2003 amendment, the Centers for Medicare & Medicaid Services (CMS), the federal agency charged with administering the Medicare program, provides that "individuals/entities engaged in a business, trade, or profession are self-insured to the extent they have not purchased liability insurance coverage. This includes responsibility for deductibles. " 3 Thus, a business that pays a settlement or judgment, including any deductible or co-pay, to a tort claimant is deemed to be self-insured, even if the business can obtain reimbursement for some or all of its payment later from an insurer.
Can you be sued for Medicare liens?
Normally, both Medicare and Medicaid have liens on any such recovery. You will need a lawyer to deal with the complicated subrogation issues and protect any recovery you receive. If you fail to properly report the recovery then you can be sued by the government...
Does Medicare pay for auto accident medical bills?
If Medicare or Medicaid has paid any of your auto-accident-related medical bills, each program has a federal lien against your recovery. You are obligated to satisfy that lien. The adverse insurance carrier also has liability to see to it that the lien is satisfied. If you have an attorney, your attorney should be fully aware ...
What is slide 17 of 38?
Slide 17 of 38 - Liability Insurance (including Self-Insurance) Slide notes When payments are made by sponsors of clinical trials for complications or injuries arising out of the trials , such payments are considered to be payments by liability insurance ( including self-insurance) and must be reported. The appropriate RRE should report the date that the injury/complication first arose as the date of incident. The situation should also be reported as one involving ORM.
Is PIP a no fault policy?
Slide 15 of 38 - No-Fault Slide notes Accident & Health, Short Term Travel and Occupational Accident Products are considered no-fault insurance by CMS and reportable as such under Section 111. Med Pay and Personal Injury Protection (PIP) are both considered no-fault insurance by CMS. RREs must combine PIP/Med Pay limits for one policy when they are separate coverages and being paid out on claims for the same injured party and same incident under a single policy and not terminate the ORM until both the PIP and Med Pay limits are exhausted. If PIP and Med Pay are coverages under separate policies, then separate records with the applicable no-fault policy limits for each should be reported.
Can an RRE submit more than one record?
Consequently, it is possible that an RRE will submit more than one record for a particular individual in a particular quarter’s Claim Input File.
Is Medicare a secondary insurance?
Slide 23 of 38 - Policies or Self-Insurance Which Allege they are Supplemental to Medicare Slide notes By statute, Medicare is secondary to liability insurance (including self-insurance), no-fault insurance, and workers’ compensation. An insurer or self-insured entity cannot, by contract or otherwise, supersede federal law.
How long does it take to report a lawsuit settlement to Medicaid?
This must be done within 10 days of receiving the settlement. After reporting, it would be advisable to contact or consult a reputable service to handle the matter. Medicaid considers assets or money from a lawsuit settlement to be income for the month it was received.
What happens if you lose your SSI?
Simply said, if an individual is receiving SSI and they lose their eligibility, they would in turn lose their Medicaid eligibility. People with Medicaid who will receive a settlement, should know how lawsuit settlements can affect Medicaid qualification.
Can a lawsuit affect medicaid?
Lawsuit settlements affect Medicaid qualification one way or another. To get the best advice and options, people on Medicaid who will receive a lawsuit settlement, should seek professional assistance. Engaging services such as Felinton’s service is the best place to start.
Is Medicaid eligibility challenging?
April 30, 2020 by Mindy Felinton. Qualifying for Medicaid is quite challenging. Persons seeking eligibility for the same can qualify through a number of methods. Unfortunately, there are various problems associated with qualifying for such programs. Medicaid has stringent resource and income limitations.
Can you lose Medicaid if you sue for a lawsuit?
If the money from a lawsuit is paid on a monthly basis, then if the amount paid is more than their Medicaid benefit, they are likely to lose their benefit for the months they will receive payment from a lawsuit settlement. Lawsuit settlements affect Medicaid qualification one way or another.
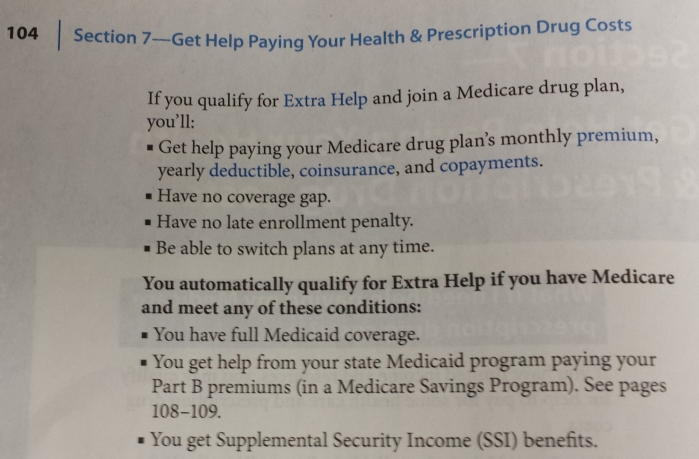
What is Medicaid?
Medicaid is a federal/state program that provides health insurance to nearly 67 million Americans. Recipients include eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. States administer Medicaid and eligibility and benefits vary by state.
Can you lose Medicaid because of an inheritance?
You could lose Medicaid coverage if you're on Medicaid and inherit money or property.
What is Medicaid estate recovery?
A state's Medicaid program may attempt to recover some Medicaid benefits after a person dies.
Can Medicaid put a lien on your property?
One way Medicaid can attempt to recover funds is to put a lien on property you own or are due to inherit.
How does Medicaid recover funds?
One way Medicaid can attempt to recover funds is to put a lien on property you own or are due to inherit. "Once a Medicaid recipient goes into a nursing home but still owns a home, Medicaid will typically put a lien on the house at that point.
Why is Medicaid important for seniors?
Tracy Craig, partner at the law firm Mirick O'Connell and chair of the firm's Trusts & Estate's group, says Medicaid is particularly helpful for seniors because it’s the only government program that pays for long-term skilled nursing home care.
What is Medicaid eligibility based on?
Medicaid eligibility is based on your monthly income and your family’s size.
What is the difference between SSI and SSDI?
SSI is different from social security disability insurance (SSDI). While SSDI also provides monthly payments to those disabled, it distinctly gives them to those who previously worked or those who have parents who work.
How to protect your SSI and Medicaid?
There are two things that you can do to protect your SSI and Medicaid benefits: Spend the settlement money in the same month on something that will not count as resources. It’s okay if you receive only a reasonable amount.
How much does Medicaid pay in Michigan?
Depending on the assessment of the Social Security Administration, the monthly payments can go as high as $771. In Michigan, Medicaid also covers those who qualify for SSI benefits. Medicaid is a healthcare program that pays for the medical expenses of persons who are disabled, elderly, young, or poor.
How much does SSI decrease?
According to the SSI program, the more you earn, the less SSI benefits you receive. For every extra dollar you earn, your SSI benefit decreases by 50 cents. It may not seem much, but you have to remember that under the SSI, you must report every income and every expense.
What is pooled trust?
Pooled trusts, on the other hand, is a trust created specifically for a non-profit association for the benefit of those disabled.
What is a pass for self support?
If you set your money aside for a Plan to Achieve Self-Support (PASS) Create a Special Needs Trust or a Pooled Trust . As a general rule, trusts are considered as a resource because, depending on the condition, you may earn something from the trust.
What is a special needs trust?
Special needs trust is a trust that contains the assets of a disabled person under the age of 65. It is established to benefit the individual, his parent, grandparent, legal guardian, or even the state should he no longer have any living beneficiary upon his death.