Full Answer
How do I submit settlement information to Medicare?
In order to submit settlement information, you must first select the injury type by clicking the radio button for the type of accident/injury/illness being claimed and/or released with respect to the Medicare beneficiary. This field is required.
What happens if I receive a settlement from Medicare?
When a beneficiary receives a settlement, judgment, award, or other payment, Medicare is entitled to recover associated payments made by the Medicare program. CMS will contact you if any additional information is needed.
How do I report a tort claim to Medicare?
Reporting a Case Medicare beneficiaries, through their attorney or otherwise, must notify Medicare when a claim is made against an alleged tortfeasor with liability insurance (including self-insurance), no-fault insurance or against Workers’ Compensation (WC).
When should I submit my notice of settlement information?
In order for Medicare to properly calculate the net refund due, settlement information must be provided. You are recommended to submit your Notice of Settlement Information as soon as the case has settled even if the settlement amount has not been received or if the funds are tied up in the registry of the courts.
Will a settlement affect my Medicare?
Since Medicare is an entitlement benefit and not a needs-based program, a client who receives legal settlement won't lose their Medicare benefits. It will not be impacted when a client receives a settlement.
Do I have to pay back Medicare?
The Nature of the Medicare Medical Lien This means that if you get a settlement, you will have to pay back Medicare before anything else gets taken out. While you can get the lien reduced, paying back Medicare after a settlement is not optional. The only path around a Medicare lien is to negotiate the lien to zero.
What is Medicare settlement?
A Workers' Compensation Medicare Set-Aside Arrangement (WCMSA) is a financial agreement that allocates a portion of a workers' compensation settlement to pay for future medical services related to the workers' compensation injury, illness, or disease.
What is the purpose of section 111 reporting?
The purpose of Section 111 reporting is to enable Medicare to correctly pay for the health insurance benefits of Medicare beneficiaries by determining primary versus secondary payer responsibility. Section 111 authorizes CMS and GHP RREs to electronically exchange health insurance benefit entitlement information.
How far back can Medicare recoup payments?
(1) Medicare contractors can begin recoupment no earlier than 41 days from the date of the initial overpayment demand but shall cease recoupment of the overpayment in question, upon receipt of a timely and valid request for a redetermination of an overpayment.
How do you qualify to get $144 back from Medicare?
To qualify for a premium reduction, you must: Be a Medicare beneficiary enrolled in Part A and Part B, Be responsible for paying the Part B premium, and. Live in a service area of a plan that has chosen to participate in this program.
Do I have to report a settlement to Medi Cal?
Medi-Cal recipients are required by law to report to the State's Department of Health Care Services any claims and lawsuits they have filed to recover compensation for their damages in a personal injury action. That report must be submitted within thirty days after a lawsuit is filed.
How is Medicare lien amount calculated?
Formula 1: Step number one: add attorney fees and costs to determine the total procurement cost. Step number two: take the total procurement cost and divide that by the gross settlement amount to determine the ratio. Step number three: multiply the lien amount by the ratio to determine the reduction amount.
What happens when Medicare denies a claim?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
How do I report to CMS?
Reporting FraudBy Phone. Health & Human Services Office of the Inspector General. 1-800-HHS-TIPS. (1-800-447-8477) ... Online. Health & Human Services Office of the Inspector General Website.By Fax. Maximum of 10 pages. 1-800-223-8164.By Mail. Office of Inspector General. ATTN: OIG HOTLINE OPERATIONS. P.O. Box 23489.
What is the reporting process of CMS?
Reporting is accomplished by either the submission of an electronic file of liability, no-fault, and workers' compensation claim information, where the injured party is a Medicare beneficiary, or by entry of this claim information directly into a secure Web portal, depending on the volume of data to be submitted.
What does CMS stand for?
Centers for Medicare & Medicaid ServicesThe Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
Why am I paying for Medicare?
Also called the hospital insurance tax, the Medicare tax helps fund the Medicare program. It's typically withheld from your taxes, according to the Internal Revenue Service.
Why do I have to pay Medicare premiums?
You must keep paying your Part B premium to keep your supplement insurance. Helps lower your share of costs for Part A and Part B services in Original Medicare. Some Medigap policies include extra benefits to lower your costs, like coverage when you travel out of the country.
Do you have to pay for Medicare out of your Social Security?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
Is Medicare Part A free at age 65?
Most people age 65 or older are eligible for free Medicare hospital insurance (Part A) if they have worked and paid Medicare taxes long enough. You can sign up for Medicare medical insurance (Part B) by paying a monthly premium. Some beneficiaries with higher incomes will pay a higher monthly Part B premium.
Provide proof of representation
Provide proof of representation After you open a case file, Medicare will send a Rights and Responsibilities letter. You will need to respond with a letter confirming your representation of the plaintiff, including a fee agreement and your client's Medicare Health Insurance Claim Number.
Review conditional payment list
Review conditional payment list Medicare will respond with a Conditional Payment letter that lists paid claims related to your client's case. Review the list carefully to determine if any unrelated payments have been included. Notify Medicare in writing if anything is amiss.
Report settlement
Report settlement When the case has been settled, report this to Medicare via letter, providing a copy of the settlement agreement and your fee agreement and list of costs. You will receive a Final Demand letter, with an updated list of payments and reductions.
How Much Will Medicare Take From My Settlement
A statute involving the Medicare lien requires anyone interested in transferring money to resolve or settle any outstanding personal injury debt. These programs also aim to provide qualified people with medical benefits.
Things To Do To Properly Address Medicare Liens
So finally, the question is what should you do in case of a personal injury settlement and medical treatment through Medicare? There are a few simple things you need to do: 1) Let your attorney know that you received treatment through Medicare, 2) Be prepared to repay Medicare, 3) Be alert to billing items unrelated to your accident, and perhaps most importantly, 4) Start early in addressing these issues..
Medicare Medicaid And Schip Of 2007
MMSEA brought us what is argued to be the most significant and most demanding reporting requirements in the history of Medicare. MMSEA requires that all entities that pay judgments to any personal injury plaintiff report the information to the Centers for Medicare and Medicaid Services .
Do You Have To Accept Whatever Amount Medicare Sends
No you dont. Keep in mind that Medicare is only entitled to reimbursement for the medical care you received as a result of the injuries you suffered in the accident. For instance, if you suffered a broken leg in the accident and then undergo treatment on the leg from January to May, you have to reimburse them for those treatments.
A Guide And Warning For Asbestos Claimants
The Stricker decision shows that insurers, attorneys and their asbestos exposure clients need to use caution when settling mesothelioma claims where there is a possibility that Medicare beneficiaries are included.
Can A Personal Injury Settlement Affect Your Eligibility For Medicare
If you are a Medicare beneficiary and are about to receive a personal injury settlement, your lawyer may have already informed you about issues that will likely arise regarding your eligibility for the program. Without careful settlement planning, you might not comply with Medicares rules and you could lose your benefits.
What Part Of My Lawsuit Settlement Can Medicare Take
Certain liens, in Illinois, hold “super lien” status. Two of these include Medicare and Medicaid. If the injured is a Medicare beneficiary and Medicare pays for the treatment, Medicare has a right to be reimbursed.
How to release information from Medicare?
Medicare does not release information from a beneficiary’s records without appropriate authorization. If you have an attorney or other representative , he or she must send the BCRC documentation that authorizes them to release information. Your attorney or other representative will receive a copy of the RAR letter and other letters from the BCRC as long as he or she has submitted a Consent to Release form. A Consent to Release (CTR) authorizes an individual or entity to receive certain information from the BCRC for a limited period of time. With that form on file, your attorney or other representative will also be sent a copy of the Conditional Payment Letter (CPL) and demand letter. If your attorney or other representative wants to enter into additional discussions with any of Medicare’s entities, you will need to submit a Proof of Representation document. A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities. If potential third-party payers submit a Consent to Release form, executed by the beneficiary, they too will receive CPLs and the demand letter. It is in the best interest of both sides to have the most accurate information available regarding the amount owed to the BCRC. Please see the following documents in the Downloads section at the bottom of this page for additional information: POR vs. CTR, Proof of Representation Model Language and Consent to Release Model Language.
What happens if a BCRC determines that another insurance is primary to Medicare?
If the BCRC determines that the other insurance is primary to Medicare, they will create an MSP occurrence and post it to Medicare’s records. If the MSP occurrence is related to an NGHP, the BCRC uses that information as well as information from CMS’ systems to identify and recover Medicare payments that should have been paid by another entity as primary payer.
What is a BCRC termination date?
The BCRC will apply a termination date (generally the date of settlement, judgment, award, or other payment ) to the case. The BCRC will identify any new, related claims that have been paid since the last time the CPL was issued up to and including the settlement/judgment/award date. Once this process is complete, the BCRC will issue a formal recovery demand letter advising you of the amount of money owed to the Medicare program. The amount of money owed is called the demand amount. The demand letter includes the following:
What is a RAR letter for MSP?
After the MSP occurrence is posted, the BCRC will send you the Rights and Responsibilities (RAR) letter. The RAR letter explains what information is needed from you and what information you can expect from the BCRC. A copy of the Rights and Responsibilities Letter can be found in the Downloads section at the bottom of this page. Please note: If Medicare is pursuing recovery directly from the insurer/workers’ compensation entity, you and your attorney or other representative will receive recovery correspondence sent to the insurer/workers’ compensation entity. For more information on insurer/workers’ compensation entity recovery, click the Insurer Non-Group Health Plan Recovery link.
How to get conditional payment information?
You can also obtain the current conditional payment amount from the BCRC or the Medicare Secondary Payer Recovery Portal (MSPRP). To obtain conditional payment information from the BCRC, call 1-855-798-2627. Click the MSPRP link for details on how to access the MSPRP.
What is conditional payment in Medicare?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
What is BCRC in Medicare?
The BCRC begins identifying claims that Medicare has paid conditionally that are related to the case, based upon details about the type of incident, illness or injury alleged. Medicare's recovery case runs from the “date of incident” through the date of settlement/judgment/award (where an “incident” involves exposure to or ingestion of a substance over time, the date of incident is the date of first exposure/ingestion).
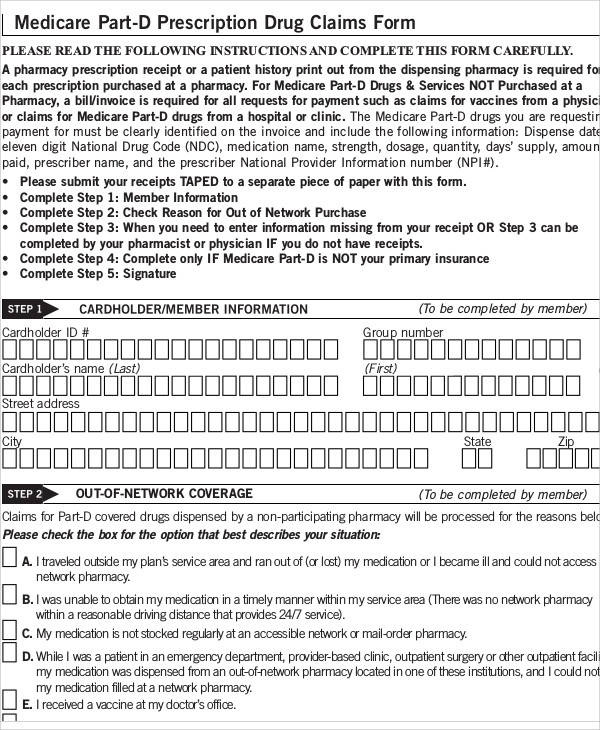
How to submit settlement information to Medicare?
In order to submit settlement information, you must first select the injury type by clicking the radio button for the type of accident/injury/illness being claimed and/or released with respect to the Medicare beneficiary. This field is required.
What is Medicare settlement amount?
The Settlement Amount is the dollar amount of the total payment obligation to or on behalf of the Medicare beneficiary in connection with the settlement, judgment, award or other payment.
When a beneficiary receives a settlement, judgment, award, or other payment, is Medicare entitled to recover?
When a beneficiary receives a settlement, judgment, award, or other payment, Medicare is entitled to recover associated payments made by the Medicare program.
What are the options for settlement?
Next is the Settlement Details section. There are four options: None, Attorney Fees, Attorney Fee Percentage or Fixed Percentage Option. If no option is selected, the settlement information will be processed without Attorney Fees.
What happens if there is no written agreement?
If there is no written agreement it is the date the payment (or first payment if there will be multiple payments) is issued.
What is settlement date?
The Settlement Date is the date the payment obligation was established, not necessarily the payment date or check issue date.
What is the Settlement Information page?
When the Provide Notice of Settlement action has been selected, the Settlement Information page displays. This page provides you with the ability to enter and submit Notice of Settlement information.
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
How long does it take to appeal a debt?
The appeal must be filed no later than 120 days from the date the demand letter is received. To file an appeal, send a letter explaining why the amount or existence of the debt is incorrect with applicable supporting documentation.
What happens if you don't respond to a debt recovery?
Failure to respond within the specified time frame may result in the initiation of additional recovery procedures, including the referral of the debt to the Department of Justice for legal action and/or the Department of the Treasury for further collection actions.
When can a WC appeal a demand?
Insurer/WC entity debtors may only appeal demands issued on or after April 28, 2015.
Does a waiver of recovery apply to a demand letter?
Note: The waiver of recovery provisions do not apply when the demand letter is issued directly to the insurer or WC entity. See Section 1870 of the Social Security Act (42 U.S.C. 1395gg).
Can an insurer appeal a WC?
The insurer/WC enti ty’s recovery agent can request an appeal for the insurer/WC entity if the insurer/WC entity has submitted an authorization, such as a Letter of Authority, for the recovery agent. Please see the Recovery Agent Authorization Model Language document which can be accessed by clicking the Insurer NGHP Recovery link.